Sexually transmitted infections affect millions of people worldwide. Many wonder if these infections will disappear naturally without treatment.
The answer depends on the specific type of STI and your body’s immune system response. Some STIs have the potential for infection resolution through natural processes. However, most require medical intervention to prevent serious complications.
Understanding which infections can self-heal versus those needing immediate treatment is crucial for your sexual wellness. This comprehensive guide ranks common STIs by their self-healing potential. You’ll learn about infection clearance rates, warning signs, and prevention strategies to protect your reproductive health.
Will STIs Go Away On Their Own? The Medical Truth Revealed
The reality about STI symptoms disappearing is complex. While some symptoms may temporarily fade, this doesn’t mean the infection is gone. Many sexually transmitted infections remain dormant in your system.
Viral STIs behave differently than bacterial ones. Your body’s natural immunity response can sometimes clear certain viral infections completely. However, most viral STIs become dormant rather than fully eliminated. Bacterial STIs rarely resolve without antibiotics.
These infections typically worsen over time if left untreated. The infection persistence factors make self-healing extremely unlikely for bacterial sexually transmitted diseases.
Disease progression varies significantly between individuals. Factors like age, overall health, and immune system strength influence treatment effectiveness rates. Never assume an infection will clear naturally without proper medical evaluation.
READ THIS BLOG : How to Grow Taller Naturally: Proven Methods That Actually Work?
HPV: The Most Common STI That Actually Clears Up Naturally
Human papillomavirus shows the highest infection clearance rate among all STIs. Studies indicate that 90% of HPV infections resolve naturally within two years. Your immune surveillance system effectively eliminates most HPV strains.
The viral shedding periods for HPV vary widely. Some people clear the virus within months, while others may take years. Young adults typically show faster clearance rates than older individuals. However, certain high-risk HPV strains can persist longer.

These persistent infections may lead to cervical cancer or other complications. Regular sexual health screening remains essential even if symptoms disappear.
Genital infection treatment for HPV focuses on symptom management rather than cure. Warts can be treated, but the virus itself must be cleared by your body’s natural defenses.
Hepatitis B Recovery: When Your Body Fights Off the Infection
Hepatitis B represents another STI that can resolve naturally. Adults with healthy immune systems clear about 95% of acute hepatitis B infections. The pathogen elimination process typically occurs within six months.
Chronic hepatitis B develops when your body cannot eliminate the virus. This happens more frequently in infants and immunocompromised individuals. The therapeutic intervention becomes necessary for chronic cases.
Reproductive health risks associated with hepatitis B include transmission to sexual partners and newborns. Even recovered individuals may carry antibodies that provide future protection.
Diagnostic accuracy for hepatitis B requires specific blood tests. These tests distinguish between acute, chronic, and recovered infections. Regular monitoring ensures proper clinical outcomes.
Herpes Reality Check: Why Symptoms Disappear But Virus Stays
Herpes simplex virus creates confusion about symptom recurrence patterns. Initial outbreaks may seem to disappear completely, leading people to believe they’re cured. Unfortunately, the virus remains dormant in nerve cells.
Dormant virus activation occurs unpredictably throughout life. Stress, illness, or immune system changes can trigger new outbreaks. The virus never truly leaves your system despite symptom-free periods.
Viral vs bacterial STIs differ significantly in their behavior. Herpes belongs to the viral category that establishes lifelong infection. Treatment adherence with antiviral medications helps manage symptoms and reduce transmission.
STI transmission rates for herpes remain high even during asymptomatic periods. This silent transmission makes partner notification and protection essential for infection control measures.
Chlamydia and Gonorrhea: Silent STIs That Never Self-Heal
Chlamydia and gonorrhea represent bacterial colonization that worsens without treatment. These infections never resolve naturally and require antibiotic intervention. Untreated STI complications can be severe and permanent.
Early signs of sexually transmitted diseases for these infections often go unnoticed. Many people experience no symptoms initially, allowing the infection to spread internally. This silent progression makes regular STI testing frequency crucial.
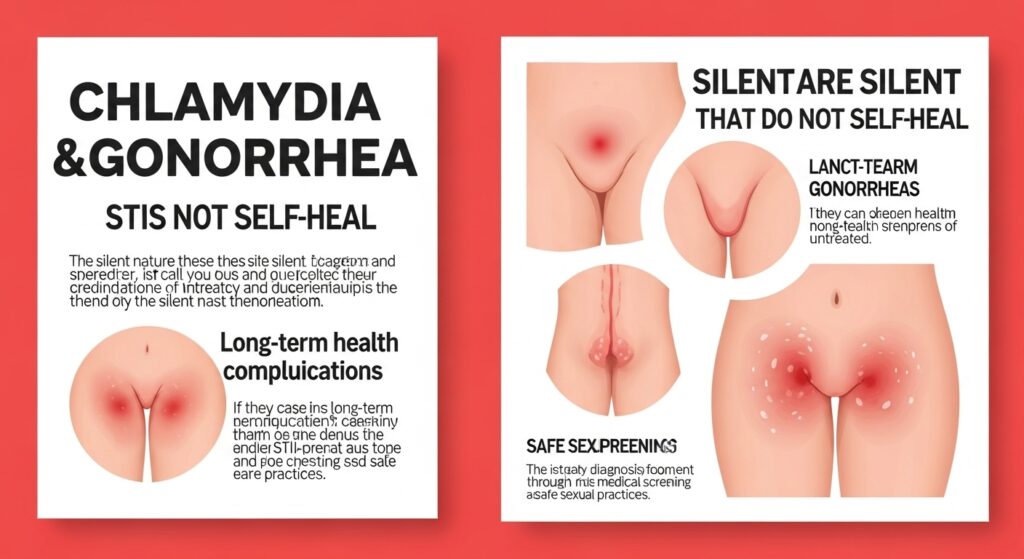
Antibiotic resistance STIs have become increasingly common. Some gonorrhea strains now resist standard treatments, requiring stronger medications. Prompt treatment prevents resistance development and reduces complications.
STI reinfection risk remains high for these bacterial infections. Previous infection provides no immunity, making prevention strategy implementation essential for sexually active individuals.
HIV and Syphilis: Life-Threatening STIs Requiring Immediate Treatment
HIV and syphilis represent the most serious STIs requiring immediate medical consultation. Neither infection ever resolves naturally, and both can be fatal without proper treatment.
HIV progression attacks your immune system systematically. Without antiretroviral therapy, the virus eventually causes AIDS. Early treatment allows people to live normal lifespans with undetectable viral loads.
Syphilis stages progress through primary, secondary, and tertiary phases. Each stage causes different symptoms and complications. Tertiary syphilis can damage the heart, brain, and other organs permanently.
Healthcare accessibility for these conditions has improved significantly. Modern treatments effectively manage both infections when started early. Regular health maintenance practices ensure optimal outcomes.
Warning Signs Your STI Hasn’t Gone Away on Its Own
Recognizing persistent STI symptoms helps distinguish between temporary relief and actual cure. How long do STI symptoms last varies by infection type and individual factors. Recurring symptoms suggest ongoing infection despite temporary improvement.
Genital discharge, pain during urination, or unusual sores indicate continued infection. These signs require immediate medical evaluation. Partner symptoms often reveal persistent infections.
If sexual partners develop symptoms, the original infection likely persists. Partner notification processes become essential for proper treatment.
Systemic symptoms like fever, fatigue, or swollen lymph nodes suggest serious complications. These warning signs indicate the infection has spread beyond the initial site.
Dangerous Complications of Leaving STIs Untreated
Untreated STI complications can affect multiple organ systems. Reproductive health risks include infertility, ectopic pregnancy, and chronic pelvic pain. These complications often prove irreversible.
Cardiovascular complications from syphilis can damage the heart and blood vessels. Neurosyphilis affects the brain and nervous system, causing dementia and paralysis. Cancer risks increase with certain untreated viral infections.
HPV causes cervical, anal, and throat cancers. Hepatitis B leads to liver cancer and cirrhosis. Pregnancy complications threaten both mother and baby. Untreated STIs can cause premature birth, low birth weight, and congenital infections in newborns.
STI Testing Guide: How to Know If You’re Really Cured?
STI testing methods vary by infection type. Blood tests detect antibodies for viral infections, while urine and swab tests identify bacterial infections. Diagnostic accuracy depends on proper timing and technique.
Confidential testing options include private clinics, health departments, and home testing kits. STI testing without insurance coverage is available through community health centers and sliding-scale programs.
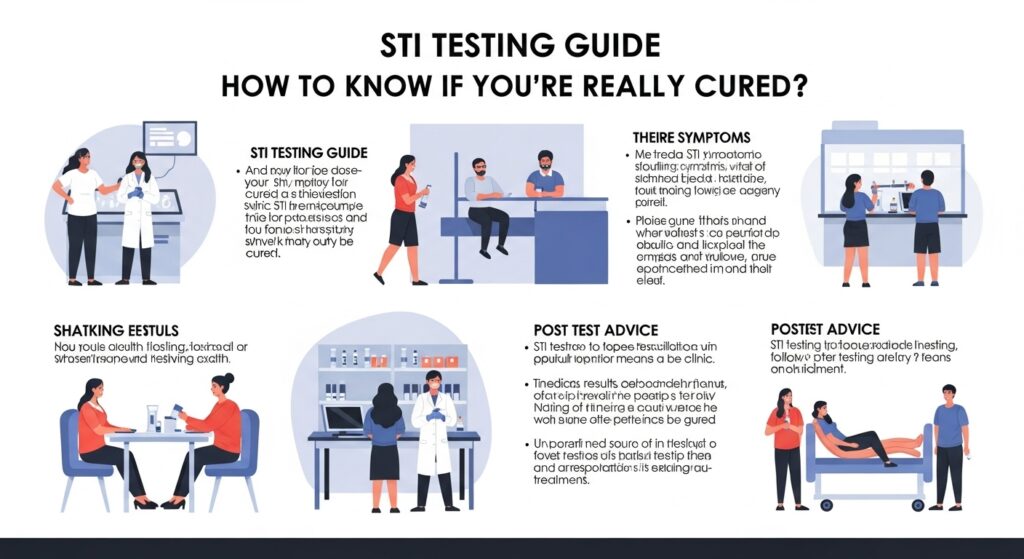
Test timing affects accuracy significantly. Testing too early may produce false negatives, while delayed testing can miss optimal treatment windows. Healthcare providers recommend specific testing schedules.
Follow-up testing confirms successful treatment for bacterial infections. Viral infections require different monitoring approaches focusing on symptom management and transmission prevention.
READ THIS BLOG : IBS Diet: Complete Guide to Foods to Eat and Avoid for Irritable Bowel Syndrome Relief
Prevention Tips: Protecting Yourself from Future STI Infections
STI prevention methods combine barrier protection, vaccination, and behavioral strategies. Contraceptive barrier methods like condoms provide excellent protection when used consistently.
Vaccination programs prevent hepatitis B and HPV infections effectively. These vaccines work best when administered before sexual activity begins. Public health initiatives promote widespread vaccination.
Sexual behavior patterns significantly influence infection risk. Limiting partners, mutual monogamy, and honest communication reduce transmission rates. STI stigma awareness encourages open discussions about sexual health.
Regular screening remains the cornerstone of prevention. Screening recommendation guidelines vary by age, gender, and risk factors. Healthcare providers customize testing schedules for individual needs.
Frequently Asked Question
Can STIs really go away without treatment?
Only HPV and hepatitis B commonly resolve naturally. Most STIs require medical treatment to prevent serious complications.
How long does it take for STIs to clear naturally?
HPV typically clears within 2 years, while hepatitis B resolves in 6 months. Other STIs don’t self-heal.
What happens if I don’t treat my STI?
Untreated STIs can cause infertility, cancer, heart damage, brain damage, and death depending on the infection type.
How often should I get tested for STIs?
Testing frequency depends on your risk factors. Most adults need annual testing, while high-risk individuals require more frequent screening.
Are there any STIs that never go away?
Herpes, HIV, and chronic hepatitis B remain lifelong infections. However, modern treatments effectively manage these conditions.
Conclusion
While some STIs like HPV and hepatitis B may resolve naturally, most sexually transmitted infections require medical treatment. The infection resolution depends on multiple factors including infection type, immune system strength, and timing of intervention. Self-healing infections represent the minority of STI cases. Relying on natural clearance risks serious complications including infertility, cancer, and death. Medical intervention necessity cannot be overstated for most sexually transmitted diseases.
Prevention strategy implementation remains more effective than treatment. Regular sexual health screening, vaccination, and safe practices protect against most STIs. Healthcare accessibility ensures everyone can receive proper care and testing. Remember that STI symptoms disappearing doesn’t guarantee cure.
David is a seasoned SEO expert with a passion for content writing, keyword research, and web development. He combines technical expertise with creative strategies to deliver exceptional digital solutions.







